*Disclaimer: All content and information in this blog is for informational and educational purposes only.
Hyperglycemia, or high blood sugar, is a common concern for people with type 1 diabetes. It occurs when the body does not have enough insulin to properly keep blood glucose levels within target range. When left untreated, hyperglycemia can lead to serious health complications such as diabetic ketoacidosis (DKA).
What is Hyperglycemia?
In people with diabetes, the body does not produce or use insulin properly, which can lead to high blood sugar levels. Hyperglycemia can be caused by a variety of factors, including eating too much sugar or carbohydrates, not getting enough physical activity, stress, illness, and certain medications. Hyperglycemia is typically defined by blood glucose levels that are >180 mg/dL 2 hours post-meal or >130 mg/dL when fasting. This reference range can vary depending on how long you’ve had diabetes, your age, and presence of other health conditions.
Symptoms of Hyperglycemia
Symptoms of hyperglycemia may include:
- Nausea
- Confusion
- Blurred vision
- Fatigue
- Dry mouth and throat
- Frequent urination
- Increased thirst
If you have type 1 diabetes and are experiencing any of these symptoms, it is important to test your blood sugar levels and take steps to bring them back to a normal range.
Hyperglycemia Treatment for Type 1 Diabetes
Treatment for hyperglycemia usually involves taking insulin to lower blood sugar levels. The amount of insulin needed will depend on a variety of factors, including the severity of the hyperglycemia, the person's age, weight, and the presence of other medical conditions.
Medication Adjustments
In some cases, a change in medication or insulin regimen may be necessary to better control blood sugar levels. This may involve adjusting the timing or dosage of insulin, or adding additional medications. It is important to work closely with a healthcare provider to develop a treatment plan that is right for you.
Monitor Blood Glucose Levels Closely
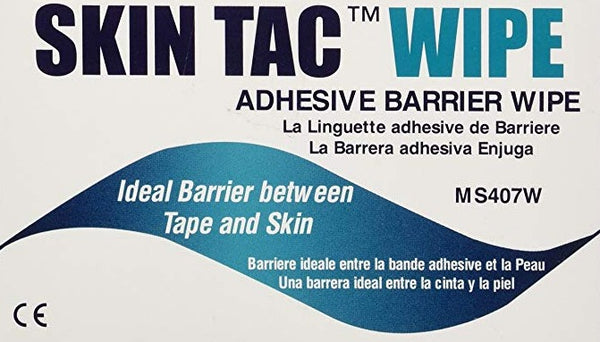
Regular monitoring of blood sugar levels can help prevent hyperglycemia and other complications of type 1 diabetes. This may involve regularly checking blood sugar levels with a glucose meter or wearing a continuous glucose monitor (CGM). CGMs are a highly effective tool to stay on top of blood sugar readings without the hassle of constant finger pricks. They are inserted onto the skin once about every 10-14 days and held on with an adhesive or tape specially made for diabetic sensors. The device continuously reads your blood sugar during that time. New models are compatible with phones and smartwatches to help you conveniently manage your blood sugar in real-time. Having accurate readings throughout the day allows you to adjust your diet, insulin, or activities to maintain a steady blood sugar that’s within a safe range.
If you do decide to use a CGM, you may be interested in our adhesive sensor patches for Freestyle Libre, Omnipod, Medtronic, and Dexcom devices. These adhesive patches are waterproof, hypoallergenic and make it easy to wear a CGM for its full lifespan while maintaining an active lifestyle. A protective patch for your CGM will let you play hard without worrying about it falling out.
Hydrate, Hydrate, Hydrate!
Hydration is important for everyone, but it is especially important for people with hyperglycemia (high blood sugar) or diabetes. Dehydration can occur when the body does not have enough fluids, and it can be especially dangerous for people with diabetes because it can affect blood sugar levels.
Hyperglycemia can cause the body to lose fluids through frequent urination, which can lead to dehydration. Dehydration can also cause blood sugar levels to rise further, leading to a vicious cycle.
It is important for people with hyperglycemia or diabetes to drink plenty of fluids, especially water, to stay hydrated. Drinking enough fluids can help to regulate blood sugar levels and prevent dehydration. It is also important to drink fluids when you are sick or have diarrhea, as these conditions can also cause dehydration.
If you are concerned about your hydration status or are experiencing symptoms of dehydration, such as thirst, dry mouth, or dizziness, it is important to talk to your healthcare provider. They can help you determine the best way to stay hydrated and manage your blood sugar levels.
Plan for Sick Days
Sick days can be especially challenging for people with type 1 diabetes. When you are sick, your body's need for insulin may change, and your blood sugar levels may be more difficult to regulate. This is because illness can cause the body to release certain hormones, such as cortisol and adrenaline, which can increase blood sugar levels.
In addition, some illnesses, such as the flu, can cause a decrease in appetite, leading to a decrease in the amount of food and carbohydrates being consumed. This can also cause blood sugar levels to rise because the body is not getting enough energy from food to match the increased demand for energy due to the illness.
It is important to pay close attention to your blood sugar levels when you are sick and take steps to bring them back to a normal range if they become too high. This may involve taking extra insulin or other medications, eating regular meals and snacks, and drinking plenty of fluids.
If you are concerned about your blood sugar levels while you are sick, it is important to talk to your healthcare provider. They can help you develop a plan to manage your blood sugar levels and provide guidance on how to adjust your insulin doses and other medications as needed.
Get Moving
Exercise is an important part of managing blood sugar levels for people with diabetes. Physical activity can help improve blood sugar control by increasing the body's sensitivity to insulin, which helps to lower blood sugar levels. It can also help to burn excess glucose, which can help to lower blood sugar levels.
However if you are experiencing hyperglycemia prior to exercise, it is important to check your ketone levels as it is generally not recommended to exercise when you have high levels of ketones in your blood or urine. Ketones are produced by the body when there is not enough insulin to use glucose as energy. When ketones build up in the body, it can lead to a condition called ketoacidosis, which can be life-threatening.
Diabetes Ketoacidosis Treatment
If you are unable to bring your blood sugar levels back to a normal range or if you are experiencing severe symptoms, it is important to seek medical attention right away. When blood sugar levels are persistently elevated, the body begins to break down fat for energy instead, which leads to the production of high levels of ketones in the blood. DKA is a medical emergency and requires immediate treatment to bring blood sugar and ketone levels back to a normal range. Treatment for DKA usually involves medical management by replenishing fluids, electrolytes, and insulin through an intravenous (IV) line.
Regular monitoring of blood sugar and ketone levels, as well as other lifestyle factors can help prevent hyperglycemia and DKA. If you are concerned about your blood sugar levels, it is important to work closely with your healthcare team to get your blood sugars as close to normal levels to reduce your risk of diabetes complications and DKA.