*Disclaimer: All content and information in this blog is for informational and educational purposes only.
This article was written by Amanda Ciprich, MS, RD. Last updated on 10/18/23.

Ozempic, victoza, trulicity and more have gained widespread popularity over the last several years. These medications fall under a class known as glucagon-like-peptide-1 receptor agonists also known as GLP-1s. They are primarily used in the management of type 2 diabetes (T2D). However, researchers have been increasingly interested in their use for chronic weight management. With a growing list of GLP-1 medications available on the market- and more on the way, it’s important to understand key aspects of this medication. Keep reading to learn more about GLP-1s and how they work.
What are GLP-1s and how do they work?
Danielle Bubliz, MS, RD from Food Freedom Diabetes explains that “GLP-1 receptor antagonists are a type of injectable medication that are used to lower blood sugars. They mimic the function of natural incretin hormones in the body to help increase insulin release with food, suppress glucagon, and slow gastric emptying.”
How to take GLP-1 medications
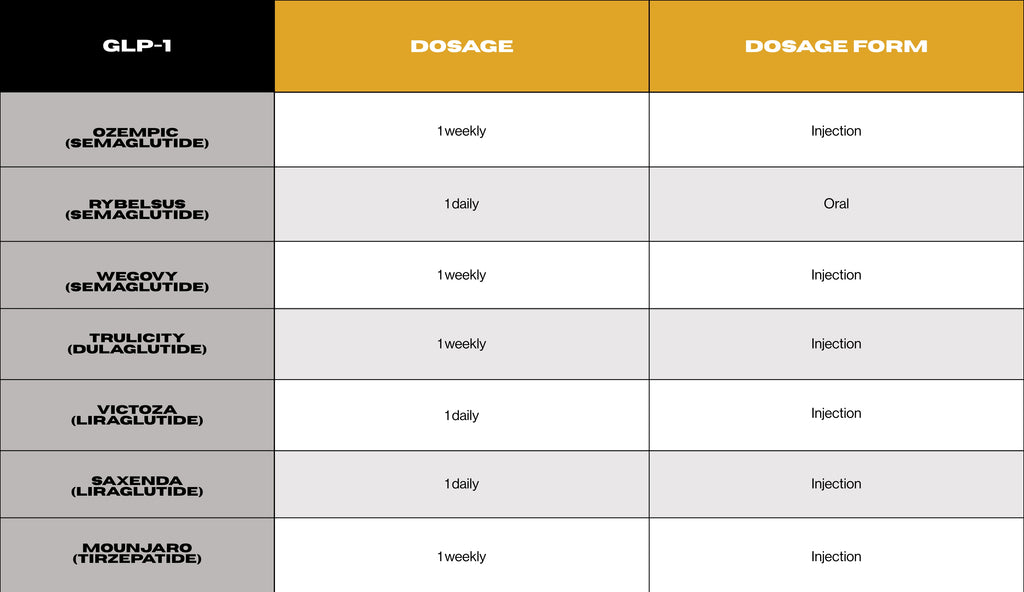
GLP-1 medications are typically self-administered through daily or weekly injections, depending on the specific medication prescribed. Rybelsus is currently the only daily oral option available in this class of medications.
GLP-1 injections should be administered into the subcutaneous fat layer just beneath the skin. Suitable injection sites include the abdomen (staying two fingers or a few inches away from the belly button), outer thighs, hips, upper buttocks, lower back, and backs of the arms.
What are the benefits of GLP-1s?
GLP-1 offers several health benefits for individuals with diabetes. Some of the key benefits include:
- A1C reduction: GLP-1s are helpful medications that can lower A1C levels in individuals with diabetes. Bubliz notes that “for those that tolerate the medication well, they can see about 0.5-1.6% reduction in their A1C.”
- Reduced risk of hypoglycemia: Unlike other blood sugar lowering medications, GLP-1s can help reduce blood sugars without increasing the risk of hypoglycemia.
- Cardiovascular benefits: Numerous studies have demonstrated that GLP-1s reduce cardiovascular risk in patients with diabetes or those at high cardiovascular risk, independent of their HbA1c levels.
- Improved kidney function: Recent developments in the management of T2D have identified the use of GLP-1s to reduce the progression of kidney disease in individuals with diabetes. Despite this beneficial effect, the exact mechanism behind how GLP-1s improve kidney function in individuals with diabetes is not fully understood at this time.
- Chronic weight management: GLP-1s have gained recent popularity for their use in chronic weight management. Bubliz explains that “GLP-1s have been helpful diabetes medications long before they became popular for weight loss.” When GLP-1s are used for chronic weight management, they require a higher effective dose compared to their use in diabetes treatment like mounjaro and wegovy,. These higher doses lead to even stronger appetite-suppressing effects, which may not be tolerated by all individuals. On average, GLP-1 use leads to a modest amount of weight loss, averaging between 5-10% of body weight, while some users may not experience any weight changes.
Keep in mind that these medications should be used alongside other lifestyle modifications, including changes to your diet and regular physical activity. Individuals interested in GLP-1s should discuss with their healthcare provider to determine whether or not they may be beneficial to you, depending on your health concerns and goals.
What are the side effects of GLP-1s?
Most GLP-1s are started at a low dose and then slowly increased to minimize potential side effects. Maja Mirkovic, MPH, RDN, CDN, CDCES, BC-ADM from In Control Nutrition reports that “the most common side effect people with diabetes can develop is nausea,” which affects between 15-45% of patients. Other common side effects of GLP-1s include a sensation of early fullness, reduced appetite, vomiting, and diarrhea.
Gastrointestinal tolerance to GLP-1s appears to vary among individuals, with some people experiencing fewer side effects than others. For some individuals, the side effects of GLP-1s tend to improve over time.
Things to consider when using GLP-1 medications
The use of GLP-1 medications are typically prescribed for individuals with T2D or chronic weight management. However, there are certain individuals and conditions who should avoid or use GLP-1s with caution. These individuals include:
- Allergy or hypersensitivity to GLP-1 medications
- Type 1 diabetes
- Pancreatitis
- Gastroparesis
- Medullary thyroid cancer
- Multiple endocrine neoplasia type 2 or family history of these conditions
- Pregnant, nursing, or trying to become pregnant
- Individuals with renal impairment
- Active eating disorder or history of disordered eating
As always, the decision to use GLP-1s should be made in consultation with a healthcare professional who can assess an individual's medical history and overall health to determine if the medication is suitable for them. It's essential to inform the healthcare provider about any pre-existing medical conditions, allergies, or medications being taken before starting GLP-1 therapy.

Commonly used GLP-1 receptor agonists:
- Ozempic (semaglutide)
- Rybelsus (semaglutide)
- Wegovy (semaglutide)
- Trulicity (dulaglutide)
- Victoza (liraglutide)
- Saxenda (liraglutide)
- Mounjaro (tirzepatide)
Which GLP-1 is best for diabetes?
The choice of which GLP-1 is best for diabetes treatment will depend on factors like patient preference with injection frequency, individual tolerance of potential side effects, overall effectiveness in managing blood sugar levels, and insurance coverage.
Can GLP-1 be used in type 1 diabetes?
GLP-1s have not received FDA approval for use in individuals with type 1 diabetes (T1D) due to concerns about increased risks of diabetic ketoacidosis and hypoglycemia associated with short-acting GLP-1s. However, long-acting GLP-1s, like victoza, trulicity and ozempic, are sometimes prescribed off-label in clinical practice for individuals with T1D. While GLP-1s have been largely studied and used for T2D, their benefits in T1D have not been explored as extensively.
While insulin therapy is the standard treatment for T1D, individuals with T1D face an elevated risk of microvascular complications, such as cardiovascular and kidney diseases. There is growing interest in exploring GLP-1 medications as promising adjunct therapies to insulin for individuals with T1D. Recent studies on long-acting GLP-1s in type 1 diabetes have shown promising results, including reductions in A1C levels and increased time within the target blood sugar range, without diabetic ketoacidosis or significant hypoglycemic episodes.It is well-established that elevated A1C levels can increase the risk of cardiovascular complications and kidney disease in individuals with T1D. These findings show that GLP-1s may hold promise as an adjunct therapy to insulin to reduce cardiovascular and kidney disease among individuals with T1D.
Additionally, there are ongoing clinical trials to further explore the effectiveness of long-acting GLP-1s in individuals with T1D and insulin resistance. These clinical trials aim to show a reduction in insulin resistance and improved glycemic management when GLP-1s are used in addition to insulin.
Overall, it's crucial to remember that the treatment of T1D is highly individualized, and healthcare providers take multiple factors into account when considering adjunct medications. People with T1D should work closely with their healthcare team to develop a personalized treatment plan that aligns with their specific needs and effectively manages their condition.
Are GLP-1s better than metformin?
Rachel Halverson, RN, CDCES, NC-BC explains that “metformin is typically considered the first-line of treatment for T2D and is widely used due to its long history of effectiveness, safety, and low cost.” It works primarily by reducing glucose production in the liver and improving the body’s insulin sensitivity. Metformin is often prescribed along with lifestyle modifications, such as adopting a healthy diet and increasing physical activity, to help lower blood glucose levels and improve overall glycemic management.
However comparing GLP-1s to metformin is not straightforward, as individual treatment plans may vary and the choice of medication can depend on various factors. The choice between metformin and GLP-1s, or any other blood sugar lowering medication, should be made based on individual factors, including the patient's medical history, lifestyle, treatment goals, and potential side effects.
In cases where metformin is not suitable or not sufficient to achieve target blood glucose levels, healthcare providers may consider adding or switching to other medications, such as GLP-1s, DPP-4 inhibitors, SGLT-2 inhibitors, or insulin. In some cases, GLP-1s may be preferred due to their additional cardiovascular benefits, however, Mirkovic notes that “GLP-1s and metformin are often used together to help manage diabetes.”
Summary
GLP-1s have gained significant popularity in recent years, with medications like Ozempic, Victoza, Trulicity, and others being widely used. Primarily prescribed for the management of T2D, these medications have also shown increased public interest in chronic weight management. They offer several benefits for individuals with diabetes, including A1C reduction, reduced risk of hypoglycemia, cardiovascular benefits, and improved kidney function. While metformin remains the first-line treatment for T2D, GLP-1s may be used in combination with metformin for additional benefits. The choice of GLP-1 medication depends on individual factors, and patients are advised to discuss their options with healthcare providers to create personalized treatment plans that effectively manage their condition. As research continues, GLP-1s hold the potential to significantly improve the lives of individuals with diabetes.






























