This article was written by Amanda Ciprich, MS, RD. Last updated on 10/31/23.

Diabetes, a chronic condition characterized by fluctuating blood sugar levels, demands continuous monitoring and precise insulin delivery. Insulin pumps can offer significant benefits in terms of convenience and accuracy for managing diabetes, but they are not immune to malfunctions, technical issues, or unforeseen circumstances. Continue reading for details on creating a personalized backup plan to provide you with a safety net and peace of mind for uninterrupted insulin delivery.
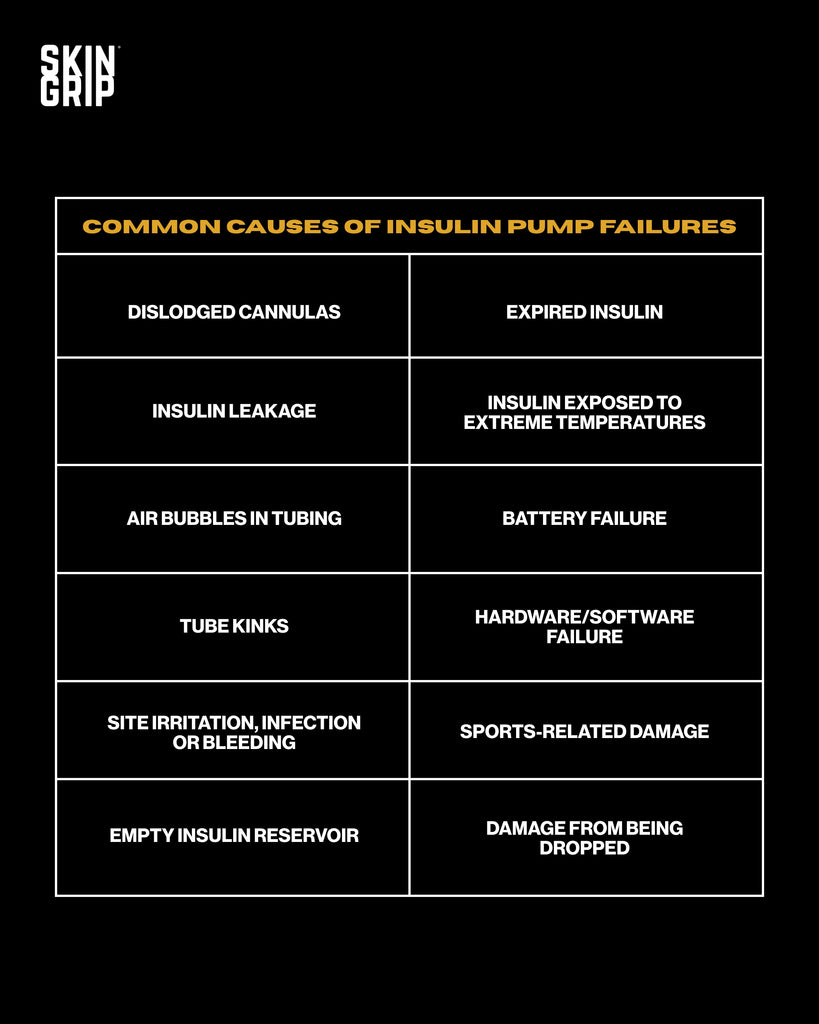
Common causes of insulin pump failures
Like any electronic device, insulin pumps can malfunction or encounter issues. Common causes for insulin pump failures includes:
- Dislodged cannulas
- Insulin leakage
- Air bubbles in tubing
- Tube kinks
- Site irritation, infection or bleeding
- Empty insulin reservoir
- Expired insulin
- Insulin exposed to extreme temperatures
- Battery failure
- Hardware/software failure
- Sports-related damage
- Damage from being dropped
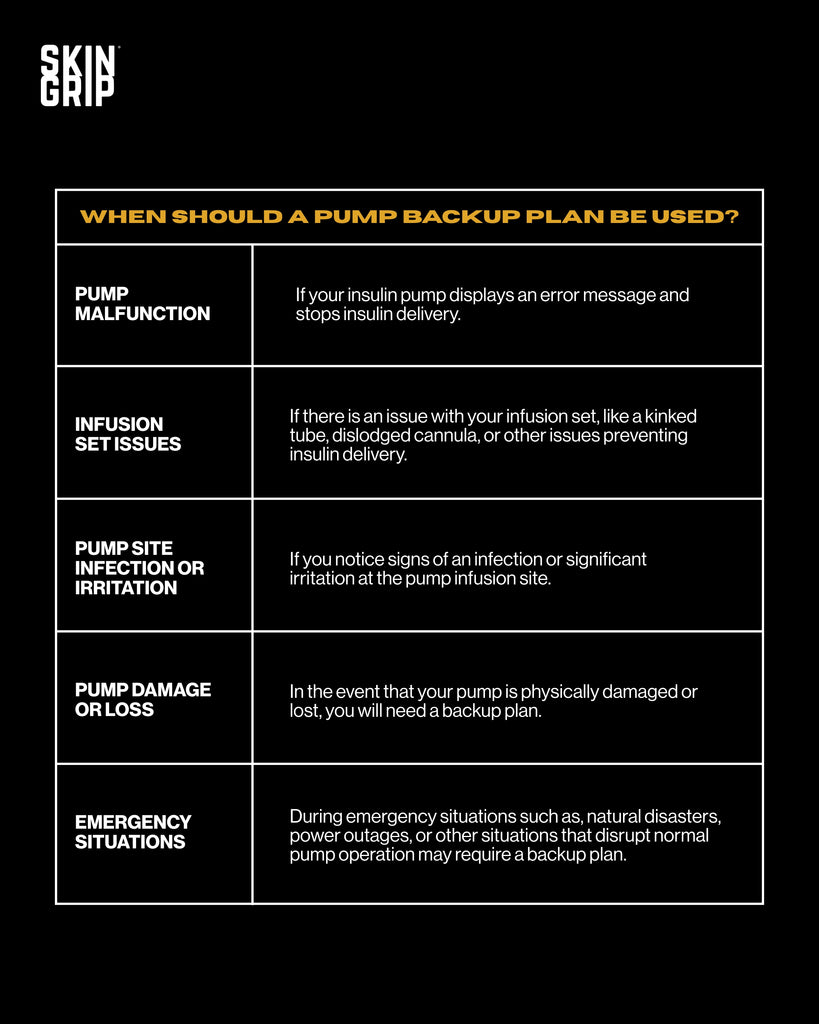
When should a pump backup plan be used
Insulin pump backup plans are crucial to ensure the continued delivery of insulin in case of pump failure or other emergencies. In these situations, it is common to observe persistent elevated blood sugar levels despite administering correction boluses through the pump alongside the presence of moderate to large ketone levels. These situations may include:
- Pump Malfunction: if your insulin pump displays an error message and stops insulin delivery.
- Infusion set issues: if there is an issue with your infusion set, like a kinked tube, dislodged cannula, or other issues preventing insulin delivery.
- Pump site infection or irritation: if you notice signs of an infection or significant irritation at the pump infusion site.
- Pump damage or loss: In the event that your pump is physically damaged or lost, you will need a backup plan.
- Emergency situations: During emergency situations such as, natural disasters, power outages, or other situations that disrupt normal pump operation may require a backup plan.
Example pump backup plans
It is important to collaborate with your healthcare team to develop a personalized insulin pump backup strategy is essential to ensure it is developed for your specific needs. Below are some general troubleshooting guidelines to consider when you find yourself without your pump for an extended period of time, ranging from several hours to several days.
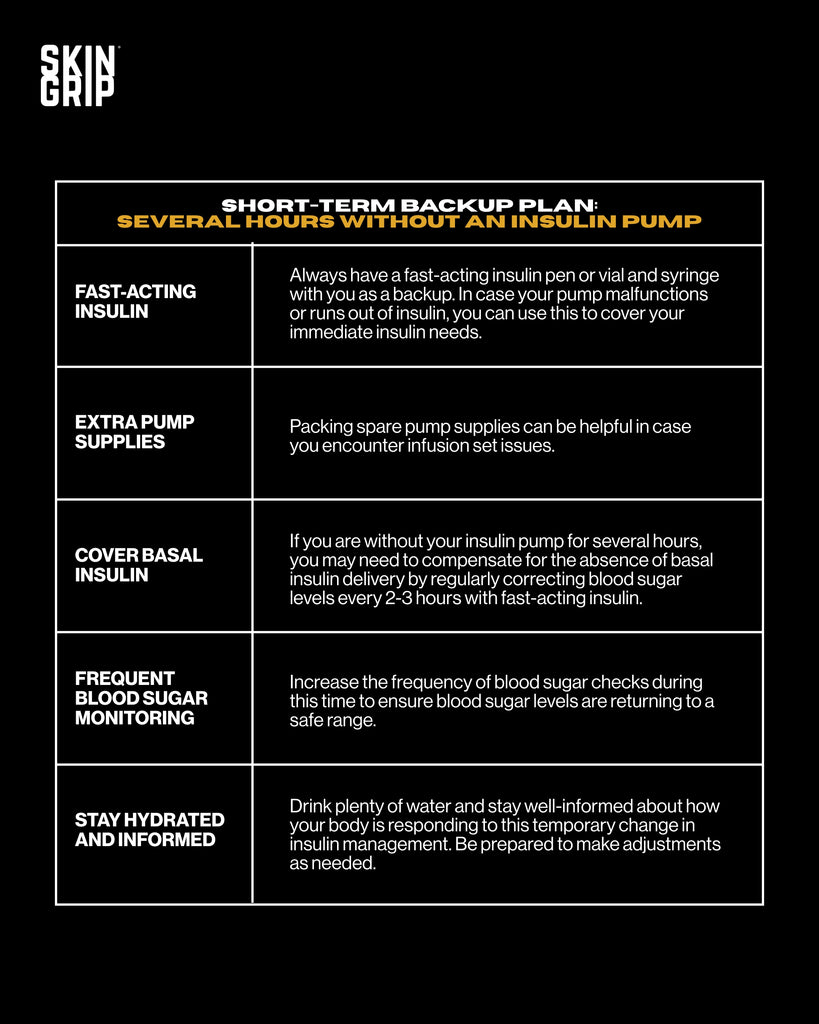
Short term backup plan: several hours without an insulin pump
In the event that you anticipate being without your insulin pump for several hours, it is essential to have a temporary backup strategy to maintain your blood sugar levels. Here is a short-term backup plan:
- Fast-acting insulin: Always have a fast-acting insulin pen or vial and syringe with you as a backup. In case your pump malfunctions or runs out of insulin, you can use this to cover your immediate insulin needs.
- Extra pump supplies: Packing spare pump supplies can be helpful in case you encounter infusion set issues.
- Cover Basal Insulin: If you are without your insulin pump for several hours, you may need to compensate for the absence of basal insulin delivery by regularly correcting blood sugar levels every 2-3 hours with fast-acting insulin.
- Frequent Blood Sugar Monitoring: Increase the frequency of blood sugar checks during this time to ensure blood sugar levels are returning to a safe range.
- Stay Hydrated and Informed: Drink plenty of water and stay well-informed about how your body is responding to this temporary change in insulin management. Be prepared to make adjustments as needed.

Long-term backup plan: several days without an insulin pump
In some situations, your insulin pump may be out of commission for several days. If this occurs, you will need a more comprehensive plan:
- Contact Manufacturer: Immediately reach out to your insulin pump manufacturer to report the issue and begin the replacement process. Most manufacturers can provide a replacement within 24-48 hours, though delays may occur.
- Obtain Long-Acting Insulin: Obtain a supply of long-acting insulin (such as Lantus) from your healthcare provider or pharmacy to fulfill your basal insulin needs, replacing the basal insulin typically delivered through your insulin pump.
- Transition to Injections: Start insulin injections following your healthcare providers recommendations for both basal and bolus insulin.
- Frequent Monitoring: Monitor your blood sugar levels closely, at least every 2-3 hours to make necessary adjustments to your insulin doses.
- Stay Connected: Maintain regular contact with your healthcare team for guidance and support throughout this period. The sudden transition from an insulin pump to injections can require more frequent medication adjustments.
Remember to engage in a discussion with your healthcare provider to create and tailor these plans based on your individual needs and situation.
What to do when your replacement insulin pump comes in
When your replacement insulin pump arrives, you should follow a series of steps to ensure a smooth transition back to your insulin pump. Here’s steps to guide you on what to do when your replacement arrives:
- Notify healthcare team: inform your healthcare provider that you have received a replacement pump. They may want to schedule an appointment or provide additional guidance based on your specific situation.
- Wait 24 hours: if you have been taking a long-acting insulin, you should wait 24 hours after the last dose before switching back to your insulin pump. If you activate your insulin pump right away, you will be receiving double your basal insulin which can result in hypoglycemia.
- Inspect the pump: carefully examine the new insulin pump to ensure that it is working without any visible defects or damage.
- Program the pump: Program your insulin pump with your specific insulin settings, including basal rates, insulin-to-carb ratios and correction factors.
- Start the pump: Begin the process of inserting the new insulin pump based on the manufacturer directions.
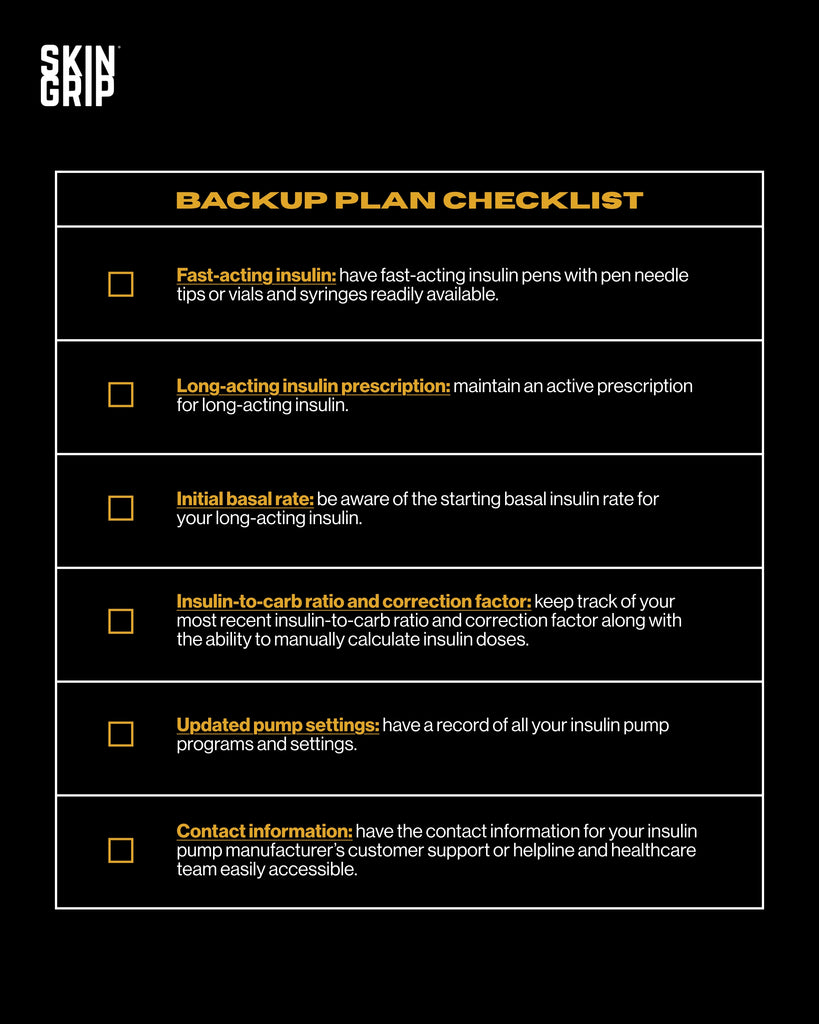
Checklist for how to be prepared for an insulin pump malfunction
Although insulin pumps offer reliability and convenience, they can still experience technical issues, or unforeseen circumstances. To ensure your insulin delivery remains uninterrupted, use this checklist to maintain preparedness and a peace of mind:
- Fast-acting insulin: have fast-acting insulin pens with pen needle tips or vials and syringes readily available.
- Long-acting insulin prescription: maintain an active prescription for long-acting insulin.
- Initial basal rate: be aware of the starting basal insulin rate for your long-acting insulin.
- Insulin-to-carb ratio and correction factor: keep track of your most recent insulin-to-carb ratio and correction factor along with the ability to manually calculate insulin doses.
- Updated pump settings: have a record of all your insulin pump programs and settings.
- Contact information: have the contact information for your insulin pump manufacturer’s customer support or helpline and healthcare team easily accessible.
Summary
While insulin pumps offer significant benefits in diabetes management, having a well-thought-out backup plan is essential to ensure continuous insulin delivery in case of unforeseen circumstances. Collaborate with your healthcare team to create a plan tailored to your unique needs so you can stay prepared for any insulin pump issues that may arise.
About Amanda Ciprich, MS, RD
Amanda Ciprich, a registered dietitian with a specialization in type 1 diabetes, was diagnosed with T1D herself at the age of 18. With her expertise and personal experience, she has authored two books, including "The Caregiver's Guide to Diabetes: Practical Advice for Caring for Your Loved One." As the founder of T1D Nutritionist, a virtual insurance-based private practice, Amanda provides counseling and guidance to individuals with T1D and their families, supporting them in effectively managing diabetes.
Shop Insulin Pump Adhesive Patches
































